|
La distrofia miotónica de tipo 1 (DM1) es una enfermedad neuromuscular rara, degenerativa y grave, que afecta a unos 90.000 europeos y que todavía no tiene ningún tratamiento efectivo disponible para los pacientes.
|
Grupo de Investigación de Excelencia
|
|
Preliminary data
📝 Open access: Sabater-Arcís et al. 2020
|
Project summary
La distrofia miotónica de tipo 1 (DM1) es una enfermedad neuromuscular rara, degenerativa y grave, que afecta a unos 90.000 europeos y que todavía no tiene ningún tratamiento efectivo disponible para los pacientes. Entre sus síntomas más característicos están la debilidad y la atrofia muscular, que junto con las arritmias cardíacas son sus principales causas de mortalidad. Es una enfermedad genética provocada por una expansión del triplete CTG en una región no codificante del gen DMPK. Aunque la mutación ocurre en DMPK, numerosas evidencias indican que la enfermedad se origina por falta de función de las proteínas MBNL, las cuales quedan anormalmente retenidas en acúmulos de transcritos DMPK mutantes en el núcleo, conocidos como foci ribonucleares. Las proteínas MBNL1 y 2 se expresan abundantemente en el músculo esquelético, donde tienen funciones parcialmente redundantes en el control del procesado (splicing) y de la poliadenilación alternativa de transcritos.
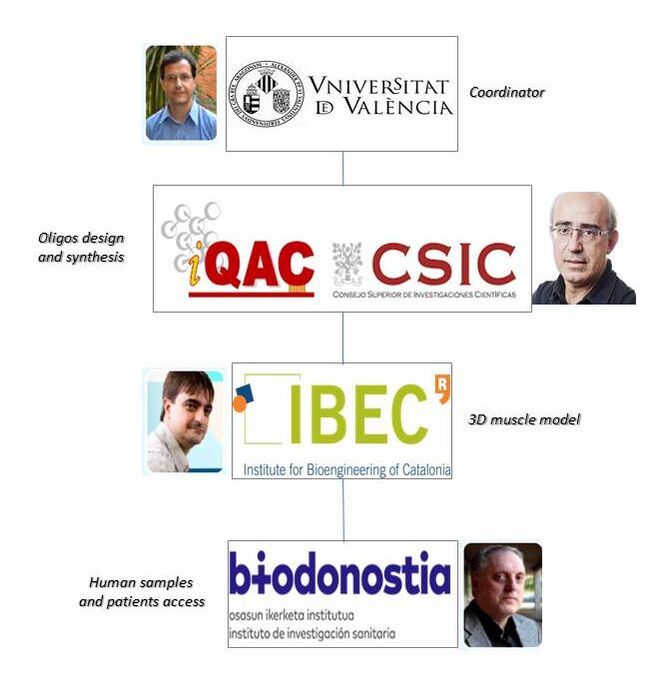
Para compensar la falta de actividad de las proteínas MBNL en DM1, previamente demostramos que se puede potenciar su expresión endógena bloqueando dos miRNAs que reprimen su traducción. Así, antagonistas de miR-23b y de miR-218 son capaces que rescatar fenotipos moleculares, celulares y funcionales en distintos modelos de la enfermedad. En paralelo observamos que estos mismos microRNAs estaban anormalmente sobreexpresados en mioblastos y en biopsias de músculo de pacientes con DM1, a la vez que identificamos uno nuevo, miR-7, un regulador clave de proceso autofágico, significativamente infraexpresado en los mismos modelos. La línea de investigación propuesta el grupo de investigación plantea objetivos de investigación básica dirigidos a descifrar el origen y las consecuencias de los cambios en el miRNoma identificados y en relación con la enfermedad, así como objetivos traslacionales encaminados a avanzar en el desarrollo de moléculas moduladoras de la actividad de los mismos:
|
Project results published
MBNL1/2 depletion interferes with a developmental alternative splicing switch that causes the expression of fetal isoforms in adults. Boosting the endogenous expression of MBNL proteins by inhibiting the natural translational repressors miR-23b and miR-218 has previously been shown to be a promising therapeutic approach. We designed antimiRs against both miRNAs with a phosphorodiamidate morpholino oligonucleotide (PMO) chemistry conjugated to cell-penetrating peptides (CPPs) to improve delivery to affected tissues. In DM1 cells, CPP-PMOs significantly increased MBNL1 levels. In HSALR mice, intravenous injections of CPP-PMOs improve molecular, histopathological, and functional phenotypes, without signs of toxicity. Our findings place CPP-PMOs as promising antimiR candidates to overcome the treatment delivery challenge in DM1 therapy.

We previously proposed an MSI2>miR-7>autophagy signalling axis whereby MSI2 overexpression repressed miR-7 biogenesis that subsequently promotes excessive autophagy. We hypothesized that MSI2 overexpression was sufficient to promote muscle atrophy and dysfunction in vivo.
Msi2 was overexpressed in neonates mice skeletal muscle to induce DM1-like phenotypes. Sustained overexpression of the murine Msi2 protein induced autophagic flux and expression of critical autophagy proteins, increased central nuclei, reduced myofibers area, and weakened muscle strength. Importantly, these changes were independent of Mbnl1, Mbnl2, and Celf1 protein levels, which remained unchanged upon Msi2 overexpression. Globally, new data from these experiments confirm the pathological role of Msi2 expression levels as an atrophy-associated component that impacts the characteristic muscle dysfunction symptoms in DM1 patients.
Msi2 was overexpressed in neonates mice skeletal muscle to induce DM1-like phenotypes. Sustained overexpression of the murine Msi2 protein induced autophagic flux and expression of critical autophagy proteins, increased central nuclei, reduced myofibers area, and weakened muscle strength. Importantly, these changes were independent of Mbnl1, Mbnl2, and Celf1 protein levels, which remained unchanged upon Msi2 overexpression. Globally, new data from these experiments confirm the pathological role of Msi2 expression levels as an atrophy-associated component that impacts the characteristic muscle dysfunction symptoms in DM1 patients.
The beginning of the 20th decade has witnessed an increase in drug development programs for myotonic dystrophy type 1 (DM1). We have collected nearly 20 candidate drugs with accomplished preclinical and clinical phases, updating our previous drug development pipeline review with new entries and relevant milestones for pre-existing candidates. Three interventional first-in-human clinical trials got underway with distinct drug classes, namely AOC 1001 and DYNE-101 nucleic acid-based therapies, and the small molecule pitolisant, which joins the race toward market authorization with other repurposed drugs, including tideglusib, metformin, or mexiletine, already in clinical evaluation. Furthermore, newly disclosed promising preclinical data for several additional nucleic-acid therapeutic candidates and a CRISPR-based approach, as well as the advent into the pipeline of novel therapeutic programs, increase the plausibility of success in the demanding task of providing valid treatments to patients with DM1.
Omics studies are crucial to improve our understanding of DM1. Employing tissue samples and cell lines derived from patients and animal models, omics approaches have revealed the myriad alterations in gene and microRNA expression, alternative splicing, 3' polyadenylation, CpG methylation, and proteins levels, among others, that contribute to this complex multisystem disease. In addition, omics characterization of drug candidate treatment experiments provides crucial insight into the degree of therapeutic rescue and off-target effects that can be achieved. Finally, several innovative technologies such as single-cell sequencing and artificial intelligence will have a significant impact on future DM1 research.
Myotonic dystrophy type 1 phenotypes are caused by muscleblind-like (MBNL) protein sequestration by toxic RNA in the DM1 protein kinase (DMPK) gene. DM1 patients exhibit a pathogenic number of repetitions in DMPK, which leads to downstream symptoms. Another disease characteristic is altered microRNA (miRNA) expression. Antisense oligonucleotide (AON) treatment targeting this miRNA can improve disease symptoms. Here, we present a refinement of this strategy targeting a miR-23b binding site on the MBNL1 3ʹ UTR in DM1 model cells and mice by using blockmiRs. They produce an increase in MBNL1 protein in DM1 model cells and HSA[LR] mice, and thus an increase in muscle strength and splicing and histological phenotypes.
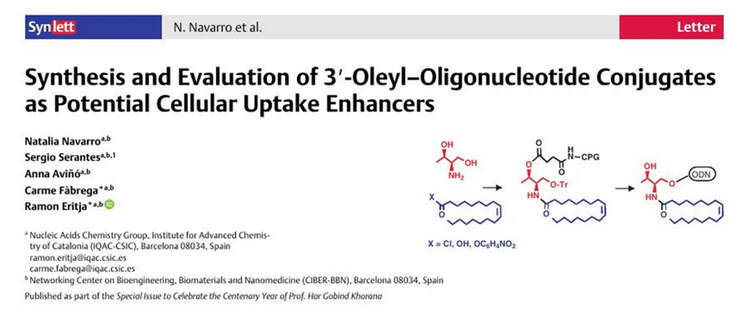
The field of therapeutic oligonucleotides has experienced significant growth in recent years, both in terms of approved drugs and those undergoing clinical trials. This expansion has transformed it into a rapidly evolving area of research. However, their cellular internalization remains a major limitation for the clinical application of oligonucleotides. To address this limitation, we report different strategies for the synthesis of specialized solid supports for the direct synthesis of 3′-oleyl-oligonucleotides by means of an l-threoninol derivative. A series of in vitro cell experiments were conducted to evaluate the potential of this strategy for enhanced cellular uptake. The results suggest that lipid conjugation enhances cellular uptake and facilitates oligonucleotide intracellular trafficking. Given these findings, the modification of therapeutic oligonucleotides through the attachment of lipidic moieties using a threoninol linker emerges as a valuable strategy to enhance their cellular internalization.
MicroRNA (miR)-7 has been demonstrated to be necessary and sufficient to repress the autophagy pathway in cell models of DM1, but the origin of its low levels in DM1 was unknown. We have found that the RNA-binding protein Musashi-2 (MSI2) is upregulated in patient-derived myoblasts and biopsy samples and previously reported that MSI2 controls miR-7 biogenesis. Using gene-silencing strategies (small interfering RNAs [siRNAs] and gapmers) and the small molecule MSI2-inhibitor Ro 08-2750, we demonstrate that reducing MSI2 levels or activity boosts miR-7 expression, represses excessive autophagy, and downregulates atrophy-related genes of the UPS system. We also detect a significant upregulation of MBNL1 upon MSI2 silencing. Taken together, we propose MSI2 as a new therapeutic target to treat muscle dysfunction in DM1.
Myotonic dystrophy type 1 (DM1) is a multisystemic neuromuscular genetic disease with an estimated prevalence of approximately at least half a million individuals based on its vast ethnic variation. Building upon a well-known physiopathology and several proof-of-concept therapeutic approaches, herein we compile a comprehensive overview of the most recent drug development programs under preclinical and clinical evaluation. Specifically, close to two dozen drug developments, eight of which are already in clinical trials, explore a diversity of new chemical entities, drug repurposing, oligonucleotide, and gene therapy-based approaches. Of these, repurposing of tideglusib, mexiletine, or metformin appear to be therapies with the most potential to receive marketing authorization for DM1.
Muscular dystrophies are a group of highly disabling disorders that share degenerative muscle weakness and wasting as common symptoms. To date, there is not an effective cure for these diseases. In the last years, bioengineered tissues have emerged as powerful tools for preclinical studies. In this review, we summarize the recent technological advances in skeletal muscle tissue engineering. We identify several ground-breaking techniques to fabricate in vitro bioartificial muscles. Accumulating evidence shows that scaffold-based tissue engineering provides topographical cues that enhance the viability and maturation of skeletal muscle. Functional bioartificial muscles have been developed using human myoblasts. These tissues accurately responded to electrical and biological stimulation. Moreover, advanced drug screening tools can be fabricated integrating these tissues in electrical stimulation platforms. However, more work introducing patient-derived cells and integrating these tissues in microdevices is needed to promote the clinical translation of bioengineered skeletal muscle as preclinical tools for muscular dystrophies.